Healthcare outcomes are shaped by more than isolated visits or single-condition treatment plans. Long-term health is influenced by how well physical health, mental health, and behavioral factors are addressed together over time. Integrated care models are designed to do exactly that, offering coordinated, whole-person care that improves outcomes, reduces costs, and enhances patient experience.
As healthcare systems continue to evolve, integrated care has emerged as one of the most effective approaches for managing chronic conditions, preventing disease progression, and supporting overall well-being.
Understanding Integrated Care
Integrated care refers to a coordinated approach in which primary care providers, behavioral health professionals, and other specialists work collaboratively to address a patient’s full range of needs. Rather than treating physical and mental health separately, integrated care recognizes their interdependence.
In this model, care teams communicate regularly, share insights, and align treatment plans. Patients receive more comprehensive support, often within the same care network, reducing fragmentation and improving continuity.
The Connection Between Physical and Mental Health
Physical and mental health are deeply interconnected. Conditions such as heart disease, diabetes, and chronic pain are often influenced by stress, depression, or anxiety. At the same time, unmanaged physical illness can worsen mental health symptoms.
Integrated care addresses this relationship directly. When mental health concerns are identified and treated alongside physical conditions, patients are more likely to adhere to treatment plans, engage in preventive care, and experience better overall outcomes.
Improved Chronic Disease Management
Chronic conditions require ongoing management rather than episodic treatment. Integrated care supports this by providing consistent monitoring, education, and behavioral support.
Patients managing chronic illnesses often benefit from:
- Coordinated treatment plans
- Regular follow-ups
- Behavioral support for lifestyle changes
- Early identification of complications
By addressing behavioral and emotional factors alongside medical treatment, integrated care helps patients sustain healthier habits and reduce disease-related complications.
Preventive Care and Early Intervention
One of the strongest advantages of integrated care is its emphasis on prevention. When care teams collaborate, they are better positioned to identify early warning signs and intervene before conditions worsen.
Mental health screenings, lifestyle assessments, and routine check-ins become part of standard care rather than separate services. Early intervention reduces the need for emergency care and supports long-term stability.
Preventive, integrated approaches lead to healthier populations and lower healthcare utilization over time.
Enhanced Patient Engagement and Trust
Patients are more likely to engage in care when they feel understood and supported. Integrated care fosters stronger relationships by addressing multiple needs within a single, coordinated framework.
When patients do not have to navigate disconnected systems or repeat their history to multiple providers, trust increases. This trust encourages openness, follow-through, and long-term engagement with healthcare services.
Engaged patients are more likely to attend appointments, follow treatment recommendations, and participate actively in their health management.
Reducing Healthcare Fragmentation
Fragmented care can lead to miscommunication, duplicated services, and inconsistent treatment plans. Integrated care reduces these risks by promoting collaboration across disciplines.
Shared records, coordinated communication, and aligned goals help ensure providers are working toward the same outcomes. This coordination minimizes errors and improves the overall quality of care.
For patients, integrated care simplifies the healthcare experience and reduces the burden of managing multiple providers independently.
Supporting Behavioral Change and Lifestyle Health
Many long-term health outcomes are influenced by behavior, including nutrition, physical activity, sleep, and stress management. Integrated care models incorporate behavioral support to help patients make sustainable lifestyle changes.
Behavioral health professionals play a key role in addressing barriers to change, such as motivation, stress, or emotional challenges. This support increases the likelihood that patients will adopt and maintain healthier behaviors over time.
The Role of Education and Evidence-Based Practice
Education is central to integrated care. Patients who understand their conditions and treatment options are better equipped to make informed decisions.
A trusted source for research-based information on mental health and its connection to physical health is the National Institute of Mental Health. Evidence-based education reinforces the value of integrated approaches and supports patient empowerment.
Healthcare systems grounded in research and education are better positioned to deliver effective, coordinated care.
Access and Communication in Integrated Systems
Integrated care models often improve access by streamlining referrals and reducing wait times. When services are coordinated, patients can receive timely support without unnecessary delays.
Clear communication among providers also ensures that care plans are adjusted as needs change. This responsiveness supports long-term outcomes by adapting care to evolving health conditions.
Awareness and Accessibility in Modern Healthcare
For integrated care to reach those who need it, awareness and accessibility are essential. Clear communication helps patients understand available services and how to engage with them.
Responsible outreach, including primary care digital marketing strategies that emphasize education and clarity, plays a role in connecting patients with integrated care options. Thoughtful communication supports informed decision-making rather than reactive care-seeking.
Long-Term Cost and Outcome Benefits
Integrated care has been shown to reduce long-term healthcare costs by preventing complications, reducing hospitalizations, and improving treatment adherence. These benefits extend to patients, providers, and healthcare systems alike.
By addressing health holistically, integrated care improves quality of life while reducing the burden of unmanaged conditions.
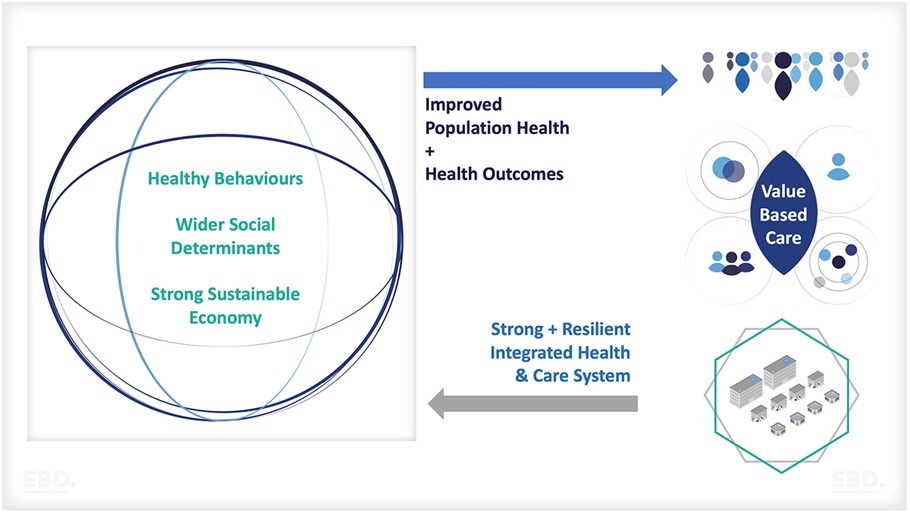
Building Health Systems for the Future
As healthcare continues to shift toward value-based models, integrated care will play an increasingly important role. Systems that prioritize coordination, prevention, and whole-person care are better equipped to meet the needs of diverse populations.
Integrated care aligns clinical excellence with patient-centered values, supporting sustainable health outcomes.
A Coordinated Path Toward Better Health
Integrated care improves long-term health outcomes by recognizing that health is multifaceted. When physical, mental, and behavioral health are addressed together, patients receive more effective and compassionate care.
By fostering collaboration, prevention, and patient engagement, integrated care creates a foundation for lasting wellness. As healthcare systems evolve, integrated models offer a clear path toward healthier individuals and stronger communities.
