Professional Dental Abscess Treatment Options
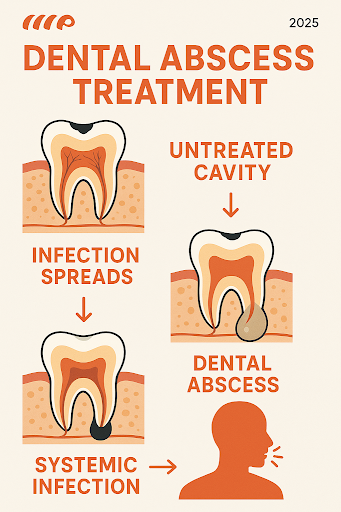
A dental abscess is a serious infection that demands professional attention. It will not resolve on its own, and delaying treatment can lead to severe complications. When you seek professional care, our primary goal is to eliminate the infection, alleviate your pain, and restore your oral health. This involves a multi-step approach, starting with an accurate diagnosis.
Diagnosis: The First Step to Relief
Before any treatment can begin, a thorough diagnosis is essential. This allows your dental professional to understand the extent of the infection, identify its source, and determine the most effective course of action. We combine a detailed patient history with a comprehensive clinical examination and advanced imaging techniques to get a complete picture.
When you present with symptoms of a dental abscess, our diagnostic process typically includes:
- Patient History and Symptom Assessment: We will ask about your symptoms, including when they started, their intensity, and what makes them better or worse. Common symptoms we look for include a persistent, throbbing toothache; sensitivity to hot or cold temperatures; pain when chewing or biting; a bitter taste in your mouth; bad breath; and general discomfort or an ill feeling. We’ll also inquire about any recent dental work, trauma, or underlying health conditions.
- Visual Inspection: Your dentist will carefully examine your mouth, teeth, and gums. We look for signs of swelling, redness, or a visible “pimple-like” bump on your gums, which indicates a pus pocket. Sometimes, the affected tooth may appear discolored.
- Palpation and Tapping Test: We may gently tap on the suspected tooth or apply pressure to the surrounding gums. A sharp increase in pain often indicates an infection at the root tip (periapical abscess). We might also palpate your neck and jaw to check for swollen lymph nodes, which are a common sign of infection spreading.
- Temperature Sensitivity Testing: Applying hot or cold stimuli to the suspected tooth can help us gauge its vitality and the extent of nerve involvement. Prolonged or severe pain in response to temperature changes often points to an infected pulp.
- Dental X-rays: This is a crucial diagnostic tool. X-rays allow us to see what’s happening beneath the surface of your gums and bone. They can reveal the presence of an abscess at the root of a tooth, bone loss around the tooth, or deep decay that has reached the pulp. For instance, a periapical abscess will often appear as a dark spot around the root tip on an X-ray, indicating bone destruction due to the infection.
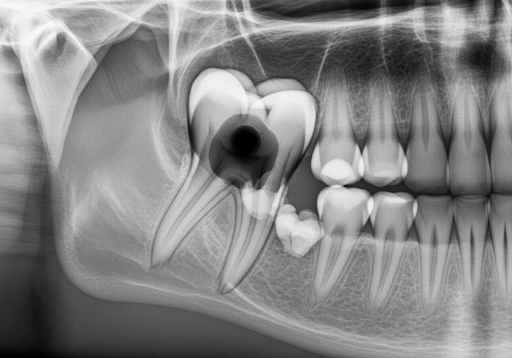
- CT Scan (Computed Tomography): In more complex cases, especially if the infection is suspected to have spread beyond the immediate tooth area or into the jawbone or surrounding soft tissues, a CT scan may be recommended. This provides a detailed, three-dimensional view, helping us accurately assess the extent of the infection and plan more intricate treatments.
By combining these diagnostic methods, we can pinpoint the source of the infection, determine the type of abscess (periapical, periodontal, or gingival), and formulate the most appropriate and effective treatment plan. This thorough approach ensures that we address the root cause of your pain and prevent further complications.
Immediate Procedures for Dental Abscess Treatment
Once a dental abscess is diagnosed, the immediate priority is to control the infection and relieve your pain. The primary method for achieving this is through drainage of the pus. This is a critical step because it reduces pressure, removes the source of bacterial toxins, and allows the body’s immune system to begin the healing process.
Here’s what typically happens during the immediate treatment phase:
- Incision and Drainage (I&D): This is often the first and most crucial step. Under local anesthesia, your dentist will make a small incision in the swollen area of the gum to allow the pus to drain. This provides immediate relief from the intense pressure and pain. The area may then be gently irrigated with a saline solution to help flush out the remaining pus and debris. In some cases, a small rubber drain might be inserted to keep the incision open and allow for continued drainage over a few days. This procedure is performed with precision and care to ensure maximum effectiveness and minimal discomfort.
- Local Anesthesia: To ensure your comfort during the drainage procedure, we will administer a local anesthetic to numb the affected area. This makes the process virtually painless.
- Antibiotics: While drainage is the primary treatment for a localized abscess, antibiotics may be prescribed if the infection has spread beyond the immediate area, if you have a weakened immune system, or if you show signs of systemic infection (like fever or swollen lymph nodes). Common antibiotics used for dental abscesses include penicillin, amoxicillin, metronidazole, or clindamycin, depending on the suspected bacteria and any allergies you may have. It’s crucial to take the full course of antibiotics as prescribed, even if your symptoms improve quickly, to ensure the infection is completely eradicated. The American Dental Association generally does not recommend routine antibiotic use for localized abscesses without signs of spreading infection, emphasizing that surgical drainage is the definitive treatment.
- Pain Management: Alongside the drainage and potential antibiotics, we will provide guidance on managing pain. This often includes recommendations for over-the-counter pain relievers like ibuprofen or acetaminophen.
- Saltwater Rinse: We may advise you to rinse your mouth gently with warm salt water several times a day. This helps to soothe the area, reduce inflammation, and promote drainage and healing.
- Seeking Professional Guidance: While immediate procedures like drainage provide significant relief, they are often just the first step. The underlying cause of the abscess must still be addressed to prevent recurrence. Seeking professional guidance for comprehensive dental abscess treatment is crucial for stopping the infection and ensuring long-term oral health. This initial intervention sets the stage for definitive treatment that addresses the source of the problem.
These immediate steps are designed to stabilize your condition, alleviate acute symptoms, and prepare you for the long-term solution that will prevent the abscess from returning.
Long-Term Dental Abscess Treatment: Saving Your Tooth
Once the immediate infection is controlled and pain is managed through drainage and, if necessary, antibiotics, the next phase of treatment focuses on eliminating the source of the infection and saving your tooth, if possible. The choice of long-term treatment depends on the severity of the abscess, the extent of damage to the tooth, and your overall oral health.
Here are the primary long-term treatment options:
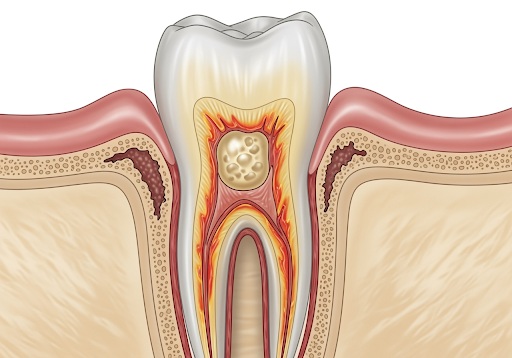
- Root Canal Therapy (Endodontic Treatment): This is the most common and preferred treatment for a periapical abscess, which originates from an infection within the tooth’s pulp. The pulp contains nerves, blood vessels, and connective tissue. When decay or trauma allows bacteria to enter the pulp, it becomes infected and eventually dies, leading to an abscess at the root tip.
- Procedure: During a root canal, your dentist or an endodontist (a root canal specialist) will remove the infected or necrotic (dead) pulp material from inside the tooth. This involves drilling a small access hole into the tooth, cleaning out the pulp chamber and root canals, and shaping them. The canals are then disinfected and filled with a biocompatible material, typically gutta-percha, to seal them and prevent future infection.
- Restoration: After the root canal, the tooth often becomes brittle because it no longer has a blood supply. To protect it from fracture and restore its function, a dental crown is usually placed over the treated tooth. A properly restored tooth after root canal treatment can last a lifetime, effectively saving your natural tooth.
- Tooth Extraction: If the tooth is too severely damaged by decay or infection to be saved with a root canal, extraction may be the only viable option. This is typically considered when:
- The tooth has extensive structural damage: such as a large crack or fracture that extends below the gum line.
- There isn’t enough healthy tooth: structure remaining to support a restoration after a root canal.
- The infection has caused: significant bone loss around the tooth, compromising its stability.
- In some cases, impacted wisdom teeth can lead to abscesses (pericoronitis), and their extraction is necessary to resolve the infection.
- Procedure: The tooth is carefully removed from its socket. Once the tooth is extracted, the infection is removed with it. The area is cleaned thoroughly to ensure no infected tissue remains.
- Replacement Options: After extraction, you’ll have options for replacing the missing tooth, such as a dental implant, a bridge, or a removable partial denture. Replacing the tooth is important to maintain proper chewing function, prevent adjacent teeth from shifting, and preserve jawbone density.
- Dental Implant: If a tooth extraction is necessary, a dental implant is often considered the gold standard for tooth replacement. An implant consists of a titanium post surgically placed into the jawbone, which acts as an artificial tooth root. Once integrated with the bone, a custom-made crown is attached to the implant, providing a stable, durable, and aesthetically pleasing replacement that functions much like a natural tooth.
- Laser Therapy for Associated Gum Disease: For periodontal abscesses, which originate in the gum tissue surrounding the tooth, treatment may involve deep cleaning procedures like scaling and root planing. In some advanced cases, laser therapy might be used to remove infected tissue and promote healing of the gum pockets. This helps to reduce inflammation and prevent the recurrence of abscesses related to gum disease.
The goal of these long-term treatments is not just to alleviate immediate symptoms but to permanently eliminate the infection’s source and preserve your oral health. We will discuss all options with you, explaining the pros and cons of each, to help you make an informed decision about the best course of action for your specific situation.
Prevention and When to Seek Emergency Care
Understanding how to prevent dental abscesses and recognizing the signs of a severe, spreading infection are critical for your overall health. While professional treatment is essential once an abscess forms, proactive measures can significantly reduce your risk, and knowing when to seek immediate medical attention can be life-saving.
At-Home Care and Pain Management (Before Your Appointment)
Experiencing the intense pain of a dental abscess can be distressing. While professional treatment is the only way to cure an abscess, there are steps you can take at home to manage the pain and discomfort while you await your dental appointment. It’s crucial to remember that these are temporary measures and do not address the underlying infection.
Here’s what you can do to find some temporary relief:
- Over-the-Counter Pain Relievers: Non-prescription pain medications can help alleviate the pain and reduce inflammation.
- Ibuprofen (e.g., Advil, Motrin): This nonsteroidal anti-inflammatory drug (NSAID) is often very effective for dental pain as it reduces both pain and swelling. Follow the dosage instructions on the package.
- Acetaminophen (e.g., Tylenol): If you cannot take ibuprofen due to medical conditions or allergies, acetaminophen is another option for pain relief.
- Combination: For adults, combining ibuprofen and acetaminophen (alternating doses) can sometimes provide more effective pain relief than either medication alone, but always consult with your dentist or pharmacist about appropriate dosages and intervals.
- Important Note: Never place aspirin directly on the tooth or gums. This can cause chemical burns and severe irritation to the soft tissues of your mouth, leading to mouth ulcers.
- Avoiding Hot and Cold Foods and Drinks: The affected tooth and surrounding area can be extremely sensitive to temperature changes. Stick to lukewarm or room-temperature foods and beverages to avoid triggering sharp pain.
- Eating Soft Foods: Chewing can put pressure on the infected tooth, exacerbating the pain. Opt for soft foods that require minimal chewing, such as soups, yogurt, mashed potatoes, scrambled eggs, and smoothies. Try to chew on the opposite side of your mouth from the affected area.
- Rinsing with Warm Salt Water: Gently rinsing your mouth with warm salt water several times a day can help soothe the inflamed tissues, draw out some of the infection, and provide temporary relief. Mix half a teaspoon of salt in a glass of warm water and swish it around your mouth for about 30 seconds before spitting it out. This can also help cleanse the area if the abscess has spontaneously ruptured.
- Elevating Your Head: When lying down, blood flow to the head can increase, intensifying the throbbing pain of an abscess. Try propping your head up with extra pillows while sleeping to reduce pressure in the area.
- Temporary Relief Only: It is vital to understand that these home remedies and pain management strategies are temporary. They will not cure the dental abscess. The infection will continue to spread and cause further damage if not professionally treated. Even if the pain subsides, it might simply mean the nerve inside the tooth has died, but the infection is still present and actively destroying tissue. This is why prompt consultation with a dental professional is paramount.
Contact your dentist as soon as possible if you suspect you have a dental abscess. Early intervention is key to preventing the infection from spreading and leading to more serious health complications.
Preventing Future Dental Abscesses
Prevention is always better than cure, especially when it comes to dental abscesses. Many abscesses stem from untreated dental caries (cavities) or gum disease. The good news is that most dental abscesses are preventable with consistent good oral hygiene practices and regular professional dental care.
Here are the best practices for preventing dental abscesses:
- Maintain Excellent Oral Hygiene: This is the cornerstone of preventing most dental problems.
- Brush Twice Daily: Brush your teeth for at least two minutes, twice a day, using a fluoride toothpaste. Fluoride helps strengthen tooth enamel and makes it more resistant to decay. Ensure you reach all surfaces of your teeth and gently brush your gum line.
- Floss Daily: Flossing or using interdental brushes once a day helps remove food particles and plaque from between your teeth and under the gum line, areas that your toothbrush can’t reach. This is crucial for preventing gum disease and cavities that can lead to abscesses.
- Don’t Rinse Immediately After Brushing: After brushing with fluoride toothpaste, spit out the excess toothpaste but avoid rinsing your mouth with water or mouthwash right away. This allows the fluoride to remain on your teeth longer, providing better protection.
- Regular Dental Check-ups and Professional Cleanings: Visit your dentist for check-ups and professional cleanings at least once every six months, or as recommended by your dentist. These visits are invaluable for:
- Early Detection: Your dentist can identify and treat small cavities before they become deep enough to infect the pulp. They can also spot early signs of gum disease.
- Professional Cleaning: Dental hygienists can remove plaque and tartar buildup that regular brushing and flossing might miss, reducing your risk of gum disease and subsequent abscesses.
- X-rays: Regular dental X-rays can reveal hidden decay or early signs of infection that aren’t visible during a clinical exam.

- Limit Sugary Foods and Drinks: Sugar feeds the bacteria in your mouth, which produce acids that erode tooth enamel and lead to cavities. Reducing your intake of sugary snacks, sodas, and juices, especially between meals, can significantly lower your risk of tooth decay. If you do consume sugary items, try to rinse your mouth with water afterward.
- Protect Your Teeth from Trauma: If you participate in sports, wear a mouthguard to protect your teeth from injury. Trauma to a tooth can damage the pulp, making it susceptible to infection and abscess formation. If you chip or crack a tooth, see your dentist immediately, as even minor damage can create an entry point for bacteria.
- Address Dry Mouth (Xerostomia): Saliva helps wash away food particles and neutralize acids. If you suffer from dry mouth (which can be caused by certain medications or medical conditions), you’re at a higher risk for tooth decay. Discuss this with your dentist or doctor, and consider using saliva substitutes or special mouth rinses.
- Avoid Tobacco Products: Smoking and chewing tobacco significantly increase your risk of gum disease, which can lead to periodontal abscesses. Quitting tobacco is one of the best things you can do for your oral and overall health.
- Manage Underlying Health Conditions: Certain medical conditions, such as diabetes, and medications that suppress the immune system can increase your susceptibility to infections, including dental abscesses. Managing these conditions effectively and informing your dentist about your full medical history is important for comprehensive care.
By adopting these preventive measures, you can dramatically reduce your chances of developing a dental abscess. Consistent care and vigilance are your best defenses against this painful and potentially dangerous condition.
Recognizing a Dental Emergency
While most dental abscesses require prompt dental attention, some situations escalate into medical emergencies that demand immediate hospital care. It’s crucial to differentiate between a severe dental issue that needs an urgent dental appointment and a life-threatening condition that requires a visit to the emergency room. Delaying care in these emergency scenarios can lead to severe, even fatal, complications.
Here are the critical signs that indicate a dental abscess has become a medical emergency:
- Severe Facial or Jaw Swelling: If the swelling from your abscess rapidly spreads to your face, jaw, neck, or even under your eye, it’s a serious concern. This indicates that the infection is moving into deeper tissues and potentially into critical areas. Swelling that makes your face appear lopsided or distorts your features is a red flag.
- High Fever and Chills: While a low-grade fever can accompany a dental abscess, a high fever (100.4°F or 38°C or higher) accompanied by chills is a strong indicator that the infection has spread systemically and is affecting your entire body. This could be a sign of sepsis, a life-threatening response to infection.
- Difficulty Breathing or Swallowing (Dysphagia/Dyspnea): This is perhaps the most alarming symptom. If the swelling in your neck or throat makes it hard to breathe, causes a muffled voice, or makes swallowing your saliva or food difficult, seek emergency medical attention immediately. The infection can spread to the deep neck spaces, potentially compressing your airway. This is a medical emergency that can lead to airway obstruction and is a primary reason for hospital admission for dental infections. The mortality rate can increase to 40% if a dental abscess leads to mediastinitis from a descending infection, highlighting the extreme danger of this complication.
- Confusion or Disorientation: If you or someone with a dental abscess becomes confused, disoriented, lethargic, or experiences changes in mental status, it could indicate that the infection has spread to the brain or is causing a severe systemic reaction. This is a neurological emergency.
- Rapid Heart Rate (Tachycardia): An liftd heart rate, especially when combined with other systemic symptoms like fever and confusion, can be a sign of severe infection or sepsis.
- Eye Involvement: If the swelling or redness spreads to your eye, causing vision changes, pain with eye movement, or difficulty opening your eye, it suggests the infection is dangerously close to your brain (e.g., cavernous sinus thrombosis), which is a rare but life-threatening complication.
- Sudden, Severe Pain Followed by Rupture and Relief (but still unwell): Sometimes, an abscess may rupture on its own, leading to a sudden release of foul-tasting pus and a temporary reduction in pain. While the pressure relief might feel good, the infection is still present and can continue to spread. If you still have a fever, swelling, or feel generally unwell after a rupture, you still need immediate professional care.
Why these symptoms are emergencies:
These symptoms indicate that the localized dental infection has progressed into a more widespread and dangerous condition. For example, dental infection admissions in hospitals occur at the rate of 1 per 2600 per population in the United States, showcasing how frequently these infections become severe enough to require hospitalization. Furthermore, approximately 47% of pediatric emergency room visits for dental issues are due to dental abscesses, emphasizing the vulnerability of children to these serious complications. Untreated tooth decay affects about 27% of adults aged 20 to 64, which is a significant risk factor for developing these severe infections.
If you experience any of these emergency signs, do not wait to see your dentist. Go to the nearest emergency room or call emergency services immediately. Inform the medical staff that you suspect a dental abscess is the underlying cause. Prompt diagnosis and treatment in an emergency setting can prevent life-threatening complications and ensure your safety. Your health and well-being are our utmost priority, and recognizing these critical signs is a vital step in protecting yourself.