Eczema continues to affect millions of individuals worldwide, presenting challenges that range from persistent itching to emotional distress. As research grows and treatment techniques evolve, patients now have more advanced options for relief than ever before. The future of eczema care is becoming brighter, with modern therapies, improved diagnostic tools, and patient centered dermatology practices leading the way. This article explores how eczema treatment is changing, what patients can expect, and how experts are shaping a more effective and personalized approach to managing this chronic skin condition.
Understanding Eczema and How the Best Eczema Doctor Approaches Care
Eczema is a long lasting inflammatory skin condition that leads to dryness, itching, redness, and recurring flare ups. It affects people of all ages and may appear in various forms such as atopic dermatitis, nummular eczema, contact dermatitis, or dyshidrotic eczema. While symptoms may differ in severity, eczema often impacts daily activities, sleep quality, and overall comfort.
The expertise of the best eczema doctor Singapore plays a vital role in identifying the root cause of flare ups and creating personalized treatment plans. Dermatologists today use advanced tools and updated clinical guidelines to manage eczema more effectively. Instead of focusing only on symptom relief, modern eczema care emphasizes long term stability, barrier repair, and minimization of triggers. Understanding these evolving approaches helps patients make informed decisions about their treatment journeys.
Types of Eczema and Their Unique Characteristics
Atopic Dermatitis
The most common form of eczema, often linked to genetics, immune response, and environmental elements. It usually begins in childhood but can occur at any age.
Contact Dermatitis
Triggered when the skin encounters irritants or allergens. Identifying and avoiding the specific trigger is essential in preventing flare ups.
Nummular Eczema
Recognized by coin shaped patches that can be intensely itchy. Moisture loss and skin injury often contribute to its development.
Dyshidrotic Eczema
Characterized by small, fluid filled blisters on the hands and feet. Stress, allergies, and humidity changes can worsen this condition.
Seborrheic Dermatitis
Typically affects oily areas such as the scalp and face. It is associated with yeast presence, skin sensitivity, and hormonal changes.
Diagnostics in Modern Dermatology
Accurate diagnosis is the foundation of effective eczema treatment. Dermatologists today rely on several methods to assess skin condition and identify contributing factors.
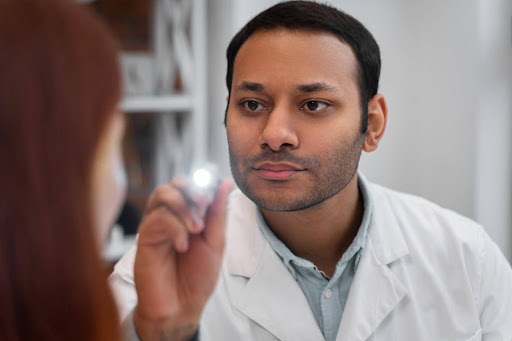
Physical Examination
A thorough skin assessment helps determine the type, location, and severity of eczema.
Medical History Review
Doctors inquire about lifestyle factors, environmental triggers, allergies, stress levels, and family history.
Allergy and Patch Testing
These tests identify sensitivities that may be fueling flare ups. Avoiding specific allergens can significantly improve symptoms.
Imaging and Skin Barrier Assessment
Some clinics use advanced imaging tools to evaluate moisture levels, inflammation, and barrier health, leading to more personalized treatment strategies.
Current and Emerging Approaches in Eczema Treatment
With new research emerging regularly, eczema care is moving beyond traditional methods. Dermatologists now offer a wider range of treatments that target both symptoms and underlying skin barrier issues.
Moisturizers and Barrier Repair Creams
These remain a fundamental part of eczema management. Newer formulas focus on ceramides, humectants, and skin repairing ingredients that strengthen the barrier.
Topical Steroids
Effective for calming inflammation, topical steroids are used during flare ups. Dermatologists emphasize proper usage to avoid side effects.
Topical Calcineurin Inhibitors
These steroid sparing options help manage sensitive areas such as the face and eyelids. They reduce inflammation and prevent flare ups.
Advanced Anti Itch Formulas
New anti itch creams provide longer relief, especially for those who prefer non steroid treatments.
Phototherapy
Controlled exposure to ultraviolet light can reduce inflammation and itching. It is an option for patients with moderate to severe eczema.
Systemic Treatments
For severe cases, oral or injectable medications targeting immune pathways may be prescribed. These options help control symptoms when topical treatments are insufficient.
Biologic Medications
One of the most significant advancements in eczema care is the development of biologics. These medications target specific parts of the immune system, improving symptoms and reducing flare ups with greater precision.
Lifestyle Centered Approaches
Dermatologists emphasize holistic care, including stress management, sleep improvement, and dietary changes that support skin health.
Daily Life Adjustments for Long Term Relief
Managing eczema involves more than clinic visits. Small lifestyle changes can significantly reduce flare ups and improve quality of life.
Hydration and Skin Moisture
Frequent moisturizing helps restore the skin barrier, reducing itching and irritation.
Gentle Skin Care
Using fragrance free cleansers, soft fabrics, and non irritating detergents can prevent unnecessary flare ups.
Stress Management
Since stress is a known trigger, practices such as deep breathing, meditation, and regular exercise are encouraged.
Environmental Control
Maintaining indoor humidity, avoiding extreme temperatures, and limiting exposure to known triggers can help keep symptoms stable.
A Clearer Path to Eczema Wellness
As research progresses, eczema care is becoming more personalized, more effective, and more patient focused. Dermatologists are combining clinical expertise, advanced treatments, and holistic strategies to support lasting skin health. With improved diagnostic accuracy and innovative therapies, the journey toward calmer, healthier skin is now more achievable.
Commonly Asked Questions
Can eczema be completely cured?
Eczema cannot be fully cured, but it can be managed effectively. Many patients achieve long periods of stability with proper care and lifestyle adjustments.
What triggers eczema flare ups?
Common triggers include allergens, temperature changes, stress, harsh skin products, and certain fabrics. Identifying triggers helps reduce flare ups significantly.
Are biologics safe for eczema treatment?
Biologic medications are generally safe and effective for moderate to severe eczema when prescribed by a qualified dermatologist. Patients undergo proper evaluation before starting these treatments.
Is eczema hereditary?
Eczema often runs in families. Genetics, environment, and immune response all play roles in its development.
How often should I see a dermatologist for eczema?
Regular visits depend on symptom severity. Patients with frequent flare ups may require more frequent follow ups, while those with stable skin may visit every few months.
Next Steps
If you experience persistent eczema symptoms or want to explore advanced treatments, consult a dermatologist who specializes in eczema care. A personalized plan based on your triggers, lifestyle, and skin needs can help you achieve calmer, healthier skin and improve long term comfort.